
The Phase I Promising Junior Investigators - 2007
Xin "Sarah" Zhang, MD; Scott M. Plafker, PhD; Zhonglin Xie, MD, PhD; Timothy J. Lyons, MD - Co-PI; Kevin R. Short, PhD;
Diane M. Warren, PhD; Jian-xing Ma, MD, PhD - PI
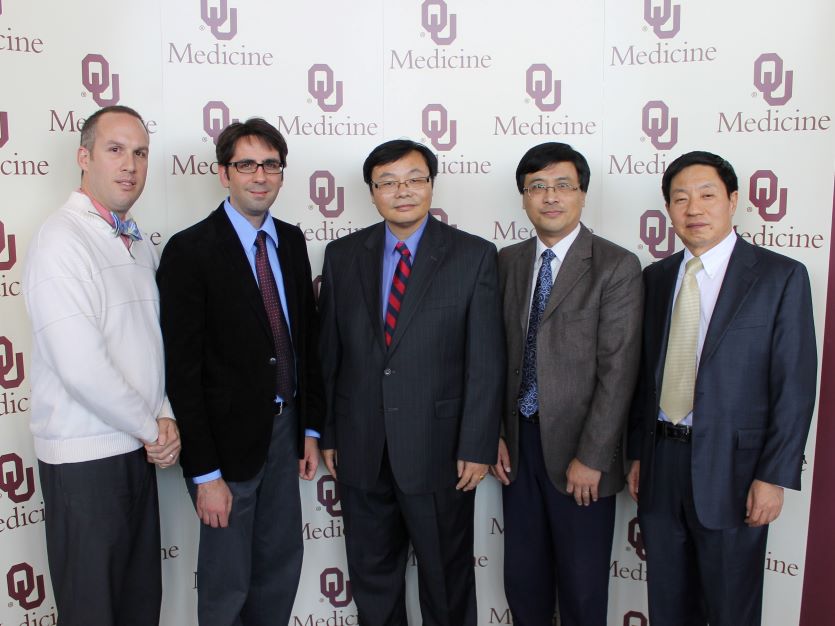
The Phase II Promising Junior Investigators - 2012
Frank Hays, Ph.D., Kenneth Humphries, Ph.D., Yun Le, Ph.D., Jian Xu, Ph.D., Jian-xing Ma, M.D., Ph.D., PI of the Diabetes CoBRE
Promising Junior Investigators
Project Title: "Effects of serum RBP4 Elevation of Endothelium and Retina"
PJI: Krysten Farjo, PhD, Mentor: Robert E. Anderson, MD PhD -Year 6-10

Krysten M. Farjo, PhD is an Assistant Professor in the Department of Physiology at the University of Oklahoma Health Sciences Center (OUHSC). She received her Ph.D. in Cell Biology from OUHSC in 2009 in the laboratory of Dr. Jian-xing Ma. Her graduate work focused on retinoid metabolism in the context of embryonic development and adult visual function. She studied a specific enzyme that is essential for embryonic development, and her work specifically deciphered its unique biochemical function in embryonic retinoic acid synthesis. In addition, she discovered that the same enzyme interacts both physically and biochemically with key components of the retinoid metabolism pathway that is necessary to initiate and sustain visual sensitivity in the adult retina. These studies were published in the specialty journals Developmental Biology and Investigative Ophthalmology and Visual Science, highlighting the impact of her work in two distinct areas of research. In 2010, within 7 months of completing her Ph.D., Dr. Farjo received her first two independent grant awards from Fight for Sight and the Oklahoma Center for the Advancement of Science and Technology (OCAST), and advanced to Assistant Professor of Research within the Department of Physiology at OUHSC. Since then, Dr. Farjo has received three additional independent research grant awards, from the American Heart Association, BrightFocus, and OCAST. She has also established an independent research program, focused on understanding the impact of increasing serum retinol-binding protein (RBP4) levels on endothelial inflammation and diabetic retinopathy. In 2013, Dr. Farjo became a tenure-track Assistant Professor, and studies in her lab have already demonstrated that elevated levels of RBP4 induce inflammation in human endothelial cells through a novel, retinol-independent mechanism. This work was published in Molecular and Cellular Biology, and serves as the foundation for current studies in her lab, which utilize RBP4-transgenic mice to study the physiological effects of increased serum RBP4 level on endothelium and retina. These studies will reveal how elevation of serum RBP4 can affect the pathophysiology of diabetic retinopathy, and could foster development of new diagnostics and therapeutics for diabetic patients.
Project Title: " ROS signaling on heart development and function"
PJI: Hui-Ying Lim, PhD, Mentor: Luke Szweda, PhD -Year 10

Hui-Ying Lim, Ph.D. is an Assistant Professor in the Department of Physiology at the University of Oklahoma Health Sciences Center (OUHSC). Dr. Lim has been studying the molecular mechanisms of diseases for more than a decade, using Drosophila as an experimental model. First as a graduate student in Dr. Andrew Tomlinson’s laboratory at Columbia University, she used the fly eye to define the processes of cell specification, an understanding that can be used to direct the generation of human retinal cell types required for vision restoration therapies. Upon graduation in 2006, she joined the laboratory of Dr. Rolf Bodmer at the Sanford-Burnham Medical Research Institute in San Diego, where she studied the paracrine role of physiological reactive oxygen species (ROS) signaling on cardiac development and function. Her work was funded by two independent American Heart Association postdoctoral fellowships awarded to Dr. Lim as a principal investigator at that time. Another study that Dr. Lim embarked on during her postdoctoral course was to investigate how dysregulation of phospholipid homeostasis could contribute to the development of lipotoxic cardiomyopathy in the fly heart. In 2011, Dr. Lim joined the Oklahoma Medical Research Foundation (OMRF) as an Assistant Member. During her term at OMRF, Dr. Lim received several awards, including the National Scientist Development Grant from the American Heart Association and an R01 award from the National Heart, Lung, and Blood Institute. In 2016, Dr. Lim moved her laboratory from OMRF to OUHSC. The overall goal of the research in her laboratory is to understand the molecular genetic mechanisms that govern cardiac physiology and energy metabolism. Specifically her laboratory is focused on (1) ROS-based paracrine signaling on cardiac physiology and pathophysiology, (2) Novel roles of genes in the pathogenesis of diet-induced obesity and diabetes. In the first research direction (1), her team investigates a novel signaling pathway mediated by physiological ROS that underlie the functional interaction between myocytes and nonmyocytes in the fly heart. In the second research direction (2), her team investigates a number of novel genes that could regulate lipid and glucose metabolism in Drosophila. For instance, they identified that the gene microsomal triglyceride transfer protein (mtp), known for its critical role in the formation of apolipoprotein B-containing lipoproteins (apoB-lipoproteins) in the fly fat body, also functions in the cardiomyocytes to regulate apoB-lipoprotein formation. Importantly, the cardiomyocyte-derived apoB-lipoproteins play a predominant role in the determinant of systemic lipid metabolism in response to high dietary fat. Together, these studies are expected to fill the knowledge gap on the poorly-understood processes - physiological ROS signaling and myocyte-nonmyocyte functional interactions, as well as contribute to the establishment of the genetic blueprint for metabolic regulation.
Project Title: "GRP78-Dependent Modulation of ER Stress Response in Diabetes"
PJI: Frank Hays, PhD, Mentor: Paul Weigel, PhD; Ann Olson, PhD -Year 6-9

Franklin A. Hays, PhD is an Assistant Professor in the Department of Biochemistry and Molecular Biology at the University of Oklahoma Health Sciences Center. He received his Ph. D. in biochemistry and biophysics from Oregon State University in 2005 in the laboratory of Dr. P. Shing Ho. Following completion of his graduate training Dr. Hays joined Dr. Robert Stroud's group at the University of California in San Francisco (UCSF) to study integral membrane protein structure and function. During this time Dr. Hays was the recipient of multiple postdoctoral fellowships, including a 3-year Ruth L. Kirschstein National Research Service Award from the NIH, and published several papers in top rated journals including Science. Dr. Hays joined the OUHSC faculty in August of 2010 and his laboratory is currently focused on understanding the underlying mechanisms of drug disposition and response in the treatment of human disease. These efforts employ a diverse array of techniques ranging from biophysical, molecular, cellular, and whole animal characterizations. Recently, Dr. Hays has initiated studies aimed at understanding how cells respond to stress within the diabetic state. This stress can be induced from numerous external stimuli, such as high blood glucose concentrations, and illicit an equally broad range of cellular response pathways. Efforts by the Hays laboratory under within this new research direction will be facilitated by interactions with established mentors on the OUHSC campus and within the Harold Hamm Oklahoma Diabetes Center.
Project Title: "Mechanisms of mitochondrial dysfunction in diabetic cardiomyopathy"
PJI: Kenneth M. Humphries, PhD, Mentor: Luke Szweda, PhD; Scott Plafker, PhD -Year 6-9

Kenneth M. Humphries, PhD is an Assistant Member at the Oklahoma Medical Research Foundation (OMRF) in the Free Radical Biology and Aging Program, and an adjunct Assistant Professor in the Departments of Biochemistry and Molecular Biology and Geriatric Medicine at the University of Oklahoma Health Science Center. Dr. Humphries received his Ph.D. from Case Western Reserve University in the Department of Physiology and Biophysics. For his graduate work, he characterized a novel mechanism of mitochondrial dysfunction induced by oxidation. This work culminated in two important papers in the journal Biochemistry that have been cited more than 350 times. Dr. Humphries did his postdoctoral work at the Howard Hughes Medical Institute, University of California San Diego, with Dr. Susan Taylor. He used this training to expand his interest in free radicals beyond their involvement in oxidative damage and into their role in redox regulation. His work at UCSD highlighted a novel aspect of cAMP-dependent protein kinase (PKA) regulation mediated by protein thiol redox status. As an independent investigator, Dr. Humphries is applying his expertise to understand how diabetes leads to increased occurrence of heart disease via changes to mitochondrial function and PKA signaling. His recent work, published in the Biochemical Journal, identified a mitochondrial modification that is elevated in diabetic heart mitochondria. This modification has implications in the prevention and treatment of a serious and deadly complication of diabetes. The results of this project will have important implications for understanding the molecular basis of diabetic cardiomyopathy.
Project Title: "VEGF Signaling in Photoreceptors."
PJI: Yun Le, PhD, Mentor: Jian-xiang Ma, MD, PhD -Year 6-8

Yun Le, PhD Diabetic retinopathy (DR) is traditionally regarded as a microvascular complication in diabetic retinas. However, it is increasingly recognized that the loss of retinal neuronal function and viability occurs before the onset of retinal microvascular abnormalities in diabetes. Diabetes induces photoreceptor degeneration. Cone degeneration is particularly devastating, as cone photoreceptors are responsible for bright and color vision. At present, the mechanisms governing diabetes-induced photoreceptor degeneration are largely unexplored. Recent studies suggest that vascular endothelial growth factor (VEGF), a major angiogenic factor that is up-regulated under hypoxic and diabetic conditions, may play a role as a survival factor for retinal neurons, including photoreceptors. However, VEGF is a therapeutic target of diabetes-induced retinal vascular complications and anti-VEGF agents have been used to develop therapeutics for DR. As VEGF receptor-2 (VEGFR2) and neuropilin-1 (NRP1) are the most abundantly expressed VEGF receptor-like proteins in neuronal cells, identifying the roles and mechanisms of VEGF signaling through VEGFR2 and NRP1 in retinal neurons is paramount to the safety of long-term anti-VEGF treatments for DR. To test our central hypothesis that VEGF signaling through VEGFR2 and NRP1 plays an essential role in preserving photoreceptor function and viability in DR, we will use both in vitro and in vivo models to determine the function and mechanisms of VEGFR2 and NRP1 signaling in photoreceptors. Experiments are designed 1) to examine VEGF/VEGFR2 signaling activated pathways, regulation of VEGFR2 activity, and the involvement of NRP1 in VEGF signaling cascade, 2) to determine if the loss of VEGFR2 exacerbates ischemia- or diabetes-induced photoreceptor dysfunction by examining cone density, retinal morphology, and photoreceptor function in rod- or cone-specific VEGFR2 knockout mice, and 3) to generate rod- or cone-specific NRP1 knockout mice and characterize photoreceptor function, morphology, and density in these conditional NRP1 knockout mice under ischemic or diabetic conditions.
Project Title: "Diabetes and the multitude of pathophysiological consequences associated with this disease state have reached epidemic proportions in the United States"
PJI: Scott M. Plafker, PhD, Mentor: Luke Szweda, PhD -Year 1-4
Scott M. Plafker, PhD received his Ph.D. from the Johns Hopkins University School of Medicine in molecular virology in the laboratory of Dr. Wade Gibson. He then did post-doctoral studies in the laboratory of Dr. Ian Macara in The Center for Cell Signaling at the University of Virginia. In Dr. Macara’s laboratory, he gained extensive experience in the field of nuclear transport and discovered a novel mechanism by which some ubiquitin pathway enzymes are imported into the nucleus. The publication of this novel mechanism in the Journal of Cell Biology was well received as reflected by its review in both Developmental Cell and Nature Cell Biology. In October of 2003, Dr. Plafker joined the Dept. of Cell Biology at the University of Oklahoma Health Sciences Center as a tenure-track Assistant Professor. His laboratory is intensively focused on defining the functional roles for different ubiquitin pathway enzymes during normal and stress states as well as during embryonic development. They currently employ a broad range of techniques and experimental systems ranging from mammalian tissue culture to the Danio rerio (zebrafish) animal model. Recently, Dr. Plafker‘s efforts have been directed towards understanding how two partner ubiquitin enzymes (UBE2E3 and RCBTB1) regulate the angiotensin II receptor during hyperglycemia. His transition into the study of ubiquitin in diabetes will be greatly facilitated by his mentor, Dr. Luke Szweda. Dr. Szweda is an Associate Member in the Free Radical Biology and Aging Research Program at the Oklahoma Medical Research Foundation (OMRF) and holds an adjunct appointment in the OUHSC Dept. of Medicine, Section of Endocrinology and Diabetes. He is a leader in the field of oxidative stress and has extensive experience using biochemical and physiological approaches to define the redox signaling mechanisms induced by diabetes. His advice and assistance with the signaling and animal studies of Dr. Plafker’s proposal will provide an ideal foundation for promoting Dr. Plafker’s development as an independent, R01-funded investigator.
Project Title: “Impact of Age and Exercise on Insulin Action”
PJI: Kevin R. Short, PhD Mentors: Kenneth C. Copeland, MD and Andrew Gardner, PhD - Year 1-4
Kevin Short, PhD obtained graduate training in human exercise physiology, metabolism and muscle biochemistry at Purdue University and Ball State University. He then completed post-doctoral work in endocrinology, diabetes, and aging at Mayo Clinic, before joining the faculty of the Mayo School of Medicine for four years. At Mayo Dr. Short developed expertise in measuring energy expenditure, protein and glucose metabolism with stable isotope-labeled tracers and tissue biochemistry in humans and animals. In 2006 Dr. Short joined the Department of Pediatrics in the Section of Diabetes and Endocrinology. Dr. Short’s current research examines the impact of exercise on insulin sensitivity and vascular health, particularly in sedentary adolescent children. The goal is to identify the most effective means to prevent or reverse the cardiometabolic risk in children and young adults, thereby limiting a potential lifetime of pathology and medical burden. The team has several years of experience in exercise physiology and has directed exercise training and metabolic outcome studies. Dr. Short and colleagues developed the new Metabolic Research Program, located in the brand new OU Children’s Physicians Building. This program goals and facilities were developed for performing clinical and basic science investigations related to the problem of obesity and diabetes in children and adolescents, with the capacity to conduct exercise testing and training, body composition, vascular function and biological sample analyses. Dr. Short’s CoBRE-supported work has examined how insulin action is affected by a single session of exercise in children versus young and elderly adults, and how different intensities of aerobic exercise training may differentially affect insulin sensitivity and vascular function in overweight sedentary adolescents. New research plans include employing exercise to reduce metabolic risk in people with spinal cord injury and measuring the impact of physical activity on the concentration and turnover of multiple cardiovascular risk proteins in circulation.
Project Title: "Impacts of central insulin on sensory coding, learning and cellular memory formation"
PJI: Lissa Tremere, PhD Mentors: Timothy J. Lyons, MD, FRCP and Raphael Pinaud, PhD -Year 4-5

Liisa Tremere, PhD conducted her PhD training in Physiology, Biophysics and Neuroscience at Dalhousie University, Canada. She has completed post-doctoral training at Oregon Health and Sciences University and Duke University. Dr. Tremere has focused her research extensively on the roles of neurohormones as neuromodulators at central sensory neurons with an emphasis on sensory processing and learning. Her work has resulted in 34 peer-reviewed publications and 2 edited books that have received favorable reviews in high impact journals, including The Lancet. Her recent work, published in the Journal of Neuroscience, provided the first demonstration that the classic female hormone estradiol, produced in the brain, is a key regulator of auditory function. This work was communicated extensively by the mainstream media in over 70 countries and became the topic of numerous scientific reviews. In September of 2010, Dr. Tremere joined the faculty of OUHSC as a tenure-track Assistant Professor. She is interested in understanding how alterations in brain neurohormonal and neurotransmitter signaling may underlie sensory processing deficits stemming from diabetes, and their association with cognitive dysfunction and dementia. Her research is extensively multi-disciplinary, ranging from genetics and molecular biology, to cellular biophysics, neurophysiological recordings in awake, behaving animals, computational and information theoretical approaches and behavioral assays in two experimental models, the songbird and mouse. Her recent efforts aim to elucidate the impact of insulin receptor signaling loss on the function of GABAA receptors, how these changes alter the central representation of sensory inputs and ultimately affect the coding and memorization of sensory experiences. An additional focus of this group is to elucidate how novel interactions between insulin receptors and signaling of membrane bound estrogen receptors contribute to memory formation of sensory events.
Dr. Tremere’s efforts on studying the effects of hormonal regulation in sensory learning will be greatly facilitated by her mentor, Dr. Raphael Pinaud. Dr. Pinaud holds the Donald W. Reynolds Endowed Chair and is a tenured Associate Professor in the Department of Physiology at OUHSC. He is recognized internationally as a leader in the field of neurohormonal regulation of sensory processing and learning in the adult brain, and is supported by multiple grants from the NIH, NSF, State and private foundations. Dr. Pinaud has worked and published extensively with Dr. Tremere, which demonstrates an already productive, successful and proven professional collaboration. In fact, Dr. Tremere and Dr. Pinaud co-published the first demonstration that neurosteroidal hormones directly controls sensory processing and learning in the adult vertebrate brain. Dr. Pinaud’s advice, assistance and unique technical and intellectual experience will ensure the successful and complete development of Dr. Tremere as an independent investigator, which will ensure her successful competition for independent, R01 level external support.
Project Title: "Genetic and environmental contributions to diabetes in Oklahoma American Indians"
PJI: Diane M. Warren, PhD Mentors: Morris W. Foster, PhD and John Mulvihill, MD; Consultant, Laura Almasy, PhD - Year 1-3
Diane Warren, PhD is an Assistant Professor in the Department of Anthropology of the University of Oklahoma. A biological anthropologist, she joined the OU faculty following a postdoctoral appointment in the Department of Genetics of the Southwest Foundation for Biomedical Research in San Antonio. At SFBR, Dr. Warren worked closely with Dr. Laura Almasy, an expert in the field of statistical genetics and a developer of SOLAR, an important software used in variance components-based analyses of data from families. Dr. Almasy will serve as a consultant to the proposed project. The focus of Dr. Warren's research at SFBR was quantitative genetic, linkage, association, and other statistical genetic analyses of complex disease phenotypes. Her research included an investigation of correlations between type 2 diabetes and hemostasis-related phenotypes. In her CoBRE application, Dr. Warren proposes to use a variance components-based approach applied to data from American Indian sib pairs to investigate the contribution of genetic, environmental, and genotype-by-environment interaction effects to variation in quantitative risk factors for type 2 diabetes. Dr. Warren will be mentored closely by Dr. Morris Foster, an anthropologist with extensive experience with research involving American Indians in Oklahoma as well as with genetic research in American Indian communities. Type 2 diabetes is a major public health concern in American Indian communities, and the results of Dr. Warren's proposed project are of potential use in the development of culturally-appropriate treatment and intervention strategies.
Project Title: "Activation of AMPK protests against diabetic vascular complications"
PJI: Zhonglin Xie, MD, PhD Mentor: Ming-Hui Zou, MD, PhD - Year 1-4
Zhonglin Xie, MD, PhD is an Assistant Professor in the Department of Medicine, Section of Endocrinology, the Oklahoma University Health Sciences Center. He received his PhD in Hokkaido University, Japan, and had an outstanding postdoctoral research experience in Boston University and University of Tennessee, during this period he was supported by a postdoctoral fellowship from the American Heart Association. Dr. Xie is very productive with over 40 publications, including 12 since 2001 in high impact journals such as Circulation, Circulation Research, Diabetes, J Biol Chem, and Hypertension. He has made the important discovery that protein kinase C- zeta regulates LKB1-AMPK cascade by increased LKB1 phosphorylation at Ser 428 and Ser 307, the latter being a newly identified phosphorylated site. His expertise in molecular biology and physiology will be applied to independent studies on the mechanisms by which AMPK activation protects against cardiovascular complications in diabetes. His studies will yield novel information of how AMPK is regulated in diabetes and if AMPK is a therapeutic target in preventing or delaying cardiovascular complications in diabetes.
Project Title: "The 26S proteasome functionality and endothelial dysfunction in diabetes."
PJI: Jian Xu, PhD, Mentor: Leonidas Tsiokas, PhD, - Year 4-8

Jian Xu, PhD is an Assistant Professor of Medicine in the Section of Endocrinology and Diabetes, Department of Internal Medicine at the University of Oklahoma Health Sciences Center (OUHSC). He received his Bachelor and Master Degree on Biochemistry and Physiology in China, his PhD degree on Biochemical Pharmacology at the University of Konstanz in Germany. He received six years of postdoctoral research training at the University of Tennessee and the University of Oklahoma Health Sciences Center. Dr. Xu has published more than 20 peer-reviewed papers in high impact-factor journals such as Circulation, Journal of Immunology, and Atherosclerosis, Thrombosis, and Vascular Biology. With support from the Department and the COBRE starting July 2010, Dr. Xu obtained a fully equipped lab space and led a research team. His lab investigates new drug targets for the treatment of vascular damage, focusing on the cause of vascular endothelial impairment and dysfunction in diabetes. His lab is the first to demonstrate alterations of 26S proteasome functionality in diabetes in vivo with a proteasome reporter mouse model. Dr. Xu has been independently funded by the American Diabetes Association, the American Heart Association and the Oklahoma Center for the Advancement of Science and Technology. His research efforts will be greatly strengthened by his COBRE mentor Dr. Leonidas Tsiokas. Dr. Tsiokas is an Associate Professor in Cell Biology at OUHSC and holds the John S. Gammill Endowed Chair in Polycystic Kidney Disease. Dr. Tsiokas’s expertise is in the area of signal transduction in Polycystic Kidney Disease and has successfully served as a mentor in a previous COBRE project. Dr. Tsiokas’ expertise in mentoring junior faculty along with his strong background in the area of signal transduction during kidney development and disease will significantly contribute to Dr. Xu’s development into a fully independent investigator.
Project Title: "Regulation of oxidative stress and inflammation in diabetic retinopathy"
PJI: Sarah Zhang, MD Mentors: Jian-xing Ma, MD, PhD, and Timothy J Lyons, MD - Year 1-3
Sarah Zhang, MD is a well-trained ophthalmologist with strong background in basic science research. She has received her Ph.D. training in China and an outstanding postdoctoral training with Dr. Jian-xing Ma, an exceptional molecular biologist in diabetes and vision research. The combination of her extensive experience in both the clinical and basic research makes Dr. Zhang an ideal candidate for independent investigator in diabetes and vision field. In nearly 10 years, she has published 42 peer-reviewed scientific articles and co-authored several review articles and book chapters. She is the first to study the anti-permeability effect of angiogenic inhibitors in diabetic retinopathy and the first to identify the novel function of pigment epithelium-derived factor (PEDF) as an endogenous anti-inflammatory factor. Her excellent work led her to be appointed as an Assistant Research Professor early this year. Recently, she has been promoted as an Assistant Professor of Medicine (tenure track). In her independent research project, Dr. Zhang will study the inhibitory effects of PEDF on oxidation, which is proposed as a central unifying mechanism for the PEDF activities of anti-inflammation, anti-permeability and neuroprotection. This unifying mechanism may explain the complex activities of PEDF in the vascular system and in retinal neurons. The success of this proposal will reveal a novel endogenous protective system in diabetic retina, and thus, identify a new pathogenic mechanism for diabetic retinopathy.