The Neonatal-Perinatal Medicine Team serves as a statewide referral center for premature and sick newborns. We average 1,400 admissions each year
Welcome to the Section of Neonatal-Perinatal Medicine at the University of Oklahoma College of Medicine. The OU Section of Neonatal-Perinatal Medicine is the only academic neonatology program in the Sooner state. We pursue excellence in Clinical Care through 24/7 in-house neonatologist coverage of a total of 107 beds including the 92 bed Level IV NICU at Oklahoma Children’s Hospital and 15 bed Level II continuing care nursery at University of Oklahoma Medical Center. Active collaboration with maternal-fetal medicine specialists in the Department of Obstetrics and Gynecology enables us to provide integrated care for high-risk pregnancies. Located within the Women’s & Newborn Center at Oklahoma Children’s Hospital, we partner with our subspecialty colleagues in Pediatric Surgery, Ophthalmology, Otolaryngology, Neurosciences, Urology, Cardiovascular Surgery, and the Department of Pediatrics to deliver coordinated care for infants with complex, life-threatening, and life-limiting conditions. Neonatal-hospitalist faculty also provide well-newborn care within Oklahoma Children’s Mother-Baby Unit. Our faculty provide community-based Level II neonatal care through partnerships with SSM Saint Anthony’s Hospital in Oklahoma City, Comanche County Memorial Hospital in Lawton, Oklahoma and Stillwater Medical in Stillwater, Oklahoma. Building on the legacy of NeoFlight, Oklahoma’s first dedicated neonatal transport service, faculty provide medical and administrative leadership for neonatal critical care transport provided through the Oklahoma Children’s Hospital Transport Program. Finally, our Telemedicine Program provides real-time consultative support to front-line providers throughout our state.
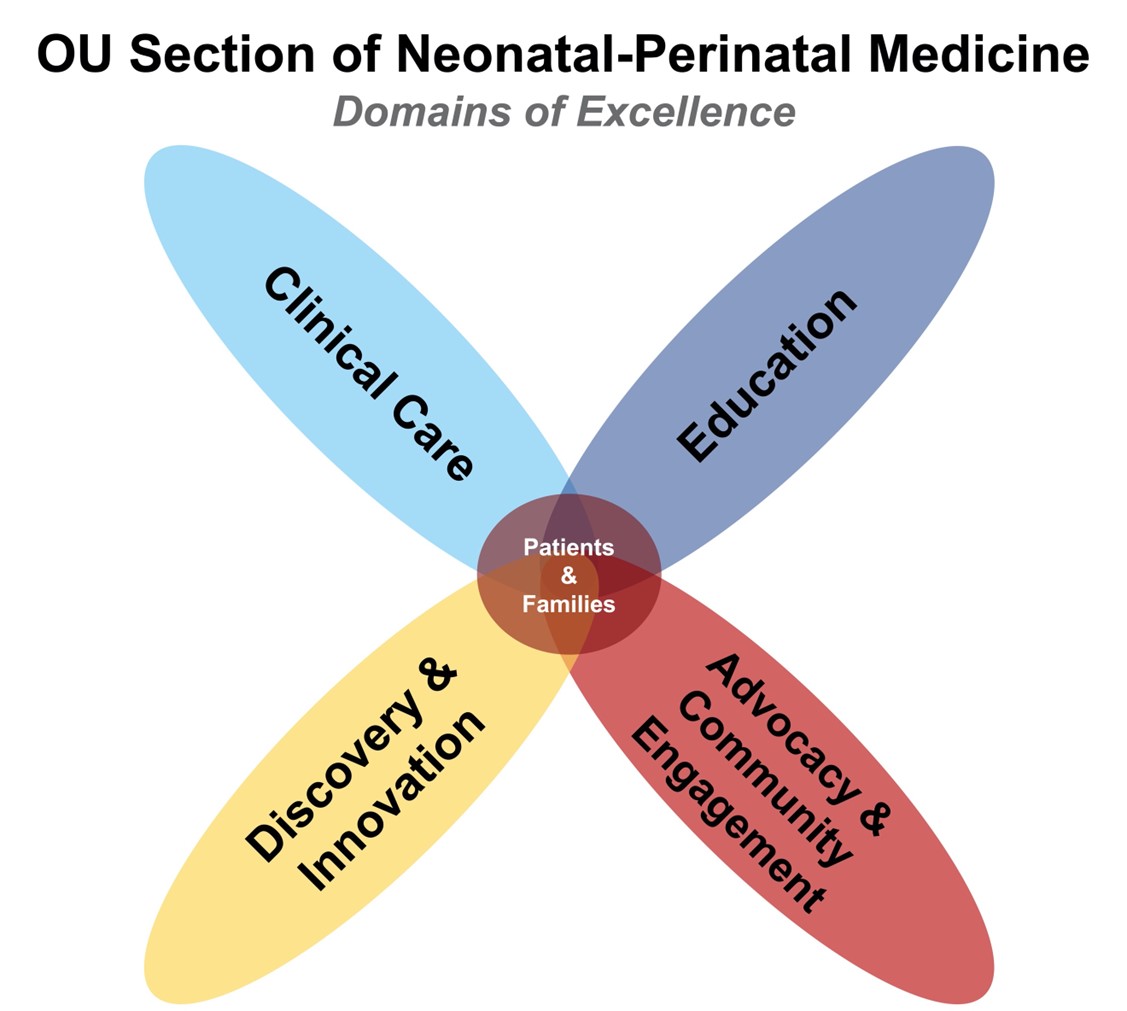 Excellence in Education within the OU Section of Neonatal-Perinatal Medicine is achieved through the training of the next generation of neonatal providers. Our Fellowship Training Program currently supports 9 trainees. The majority of neonatologists in the state of Oklahoma were trained at OUHSC. Currently under the direction of Drs. Erynn Bergner and Doug Dannaway, our trainees acquire expertise in clinical skills and patient care in the Oklahoma Children’s Hospital NICU. In addition to structured education in clinical care, quality improvement, and global health, our fellows also benefit from the robust scientific environment in our section, department, college, and campus. As one of only four centers with seven professional schools, the University of Oklahoma Health Sciences Center is the primary training site for healthcare providers in our state. Thus, our fellows benefit from this collegial and collaborative environment through active engagement with research and clinical mentors and side-by-side learning with trainees in other professional disciplines. Section faculty also serve as educators for advanced practice nursing students, physician assistant students, medical students, family medicine residents, and pediatric residents rotating through the Oklahoma Children’s Mother-Baby Unit and NICU.
Excellence in Education within the OU Section of Neonatal-Perinatal Medicine is achieved through the training of the next generation of neonatal providers. Our Fellowship Training Program currently supports 9 trainees. The majority of neonatologists in the state of Oklahoma were trained at OUHSC. Currently under the direction of Drs. Erynn Bergner and Doug Dannaway, our trainees acquire expertise in clinical skills and patient care in the Oklahoma Children’s Hospital NICU. In addition to structured education in clinical care, quality improvement, and global health, our fellows also benefit from the robust scientific environment in our section, department, college, and campus. As one of only four centers with seven professional schools, the University of Oklahoma Health Sciences Center is the primary training site for healthcare providers in our state. Thus, our fellows benefit from this collegial and collaborative environment through active engagement with research and clinical mentors and side-by-side learning with trainees in other professional disciplines. Section faculty also serve as educators for advanced practice nursing students, physician assistant students, medical students, family medicine residents, and pediatric residents rotating through the Oklahoma Children’s Mother-Baby Unit and NICU.
Discovery & Innovation occurs through laboratory-based, translational, and clinical research activities within our section. Physician and non-physician principal investigators are located within Oklahoma Children’s Hospital and the evolving Center for Pregnancy and Newborn Health at OU Research Park. This enables active engagement with emerging opportunities in the Oklahoma City Innovation District and the evolving Oklahoma City biotech environment. Section investigators are also actively engaged with the OU Office of Innovation and Corporate Partnerships to facilitate the evolution of innovative technologies through offerings such as the iPath Program. Collaborations with members of the Harold Hamm Diabetes Center, the Section of Pediatric Diabetes & Endocrinology, the Department of Nutritional Sciences, and the recently dedicated Quincy Le Norman Nutrition Center at Oklahoma Children’s Hospital will define the influences of maternal obesity/diabetes and human milk composition on outcomes in prematurely born infants. We significantly contribute to many multi-center collaborative research studies. Investigators in the Section of Neonatal-Perinatal Medicine have active research programs supported by local, regional, and national/NIH funding and provide structured research mentorship in the following themes:
- Gastrointestinal Biology
- GI Immunology
- Necrotizing Enterocolitis
- Infant Nutrition and Body Composition
- Cardiopulmonary Biology :
- Lung development, lung injury, and bronchopulmonary dysplasia
- Neonatal resuscitation education and provision
- Targeted neonal echocardiography
- Perinatal cardiovascular physiology.
- Developmental Vascular Biology:
- Retinal vascular development
- Retinopathy of prematurity.
Department of Pediatrics, OU College of Medicine, Infant Mortality Alliance and support of local refugees. Within our state, faculty serve in leadership positions in the Oklahoma Perinatal Quality Improvement Collaborative and the Oklahoma Mother’s Milk Bank. We have maintained a strong leadership presence in the Southern Society for Pediatric Research over many years. Faculty are actively contribute to our national and international scientific and educational communities by providing leadership in organizations such as the American Academy of Pediatrics (AAP) Section on Neonatal-Perinatal Medicine (SONPM), the AAP Section on Simulation and Innovative Learning Methods (SOSILM), International Liaison Committee on Resuscitation (ILCOR), Perinatal Research Society (PRS), Society for Pediatric Research (SPR), American Thoracic Society (ATS), Society for Redox Biology and Medicine (SfRBM), the Necrotizing Enterocolitis (NEC) Society, Neonatal Hemodynamics Research Center, American Pediatric Society (APS), and the American Heart Association. Clinically, section faculty are key contributors to initiatives within the Vermont-Oxford Network, Children’s Hospital Neonatal Consortium, Pan American Hemodynamics Collaborative, and the Delivery Room Intervention & Evaluation (DRIVE) Network. Finally, our annual Teleresuscitation Symposium assembles clinical and research leaders to engage with local, regional, national, and international communities to advance skills acquisition and knowledge generation.
We are proud of the work we do as Oklahoma’s flagship neonatal-perinatal medicine program and Oklahoma’s largest neonatal service line. As you review our website, I invite you to connect with us via email should you have any questions or opportunities through which we can enhance our efforts to serve the babies, families, learners, and innovators of Oklahoma and beyond.
Trent E. Tipple, M.D.
Section Chief, Neonatal-Perinatal Medicine
Children's Health Foundation Reba McEntrire Endowed Chair in Neonatology
Professor of Pediatrics
Adjunct Professor of Nutrition, Physiology, Biochemistry and Molecular Biology
University of Oklahoma Health Sciences Center
1200 North Everett Drive | Oklahoma City, OK 73104
Administrative Assistant | Shali Lay shali-lay@ouhsc.edu
405-271-5215 | Fax: 405-271-1236
Trent-Tipple@ouhsc.edu