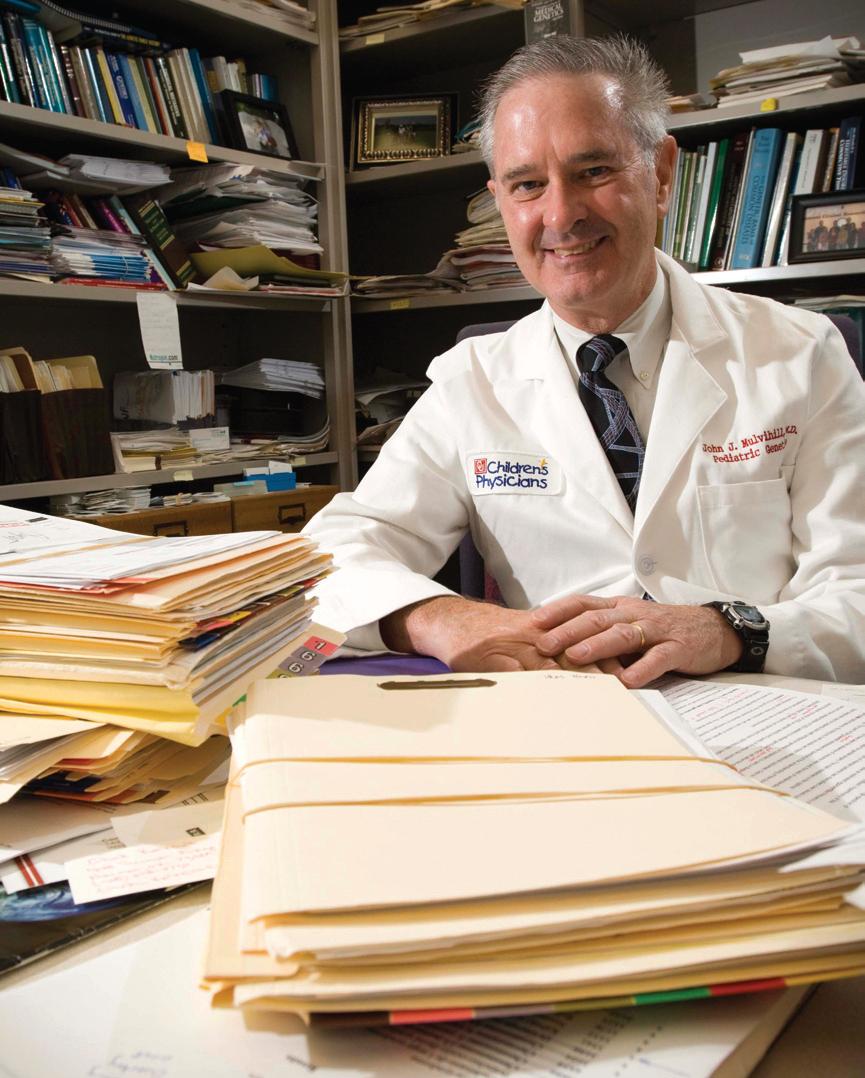
 Since earning an international reputation in the genetics of human cancer 30 years ago, John J. Mulvihill, M.D., has been chief of clinical genetics for the National Cancer Institute, founder of the human genetics department at the University of Pittsburgh and cofounder of the International Genetic Epidemiology Society. He has directed medical genetics as CMRI/Kimberly V. Talley professor of pediatrics for the OU Health Sciences Center since 1998. Although his research focus is on hereditary and familial factors and on reproduction by cancer survivors as routes to understanding human germ cell mutation, his work as a physician-scientist at OU is much more wide-ranging. Mulvihill spoke with OU Medicine Magazine about some of these issues.
Since earning an international reputation in the genetics of human cancer 30 years ago, John J. Mulvihill, M.D., has been chief of clinical genetics for the National Cancer Institute, founder of the human genetics department at the University of Pittsburgh and cofounder of the International Genetic Epidemiology Society. He has directed medical genetics as CMRI/Kimberly V. Talley professor of pediatrics for the OU Health Sciences Center since 1998. Although his research focus is on hereditary and familial factors and on reproduction by cancer survivors as routes to understanding human germ cell mutation, his work as a physician-scientist at OU is much more wide-ranging. Mulvihill spoke with OU Medicine Magazine about some of these issues.
OU Medicine: Getting right to the point, is our DNA our destiny?
Mulvihill: Nope, I'm totally against the notion that you are your DNA. Your DNA is a repository of chemicals that interact with your environment, whether it's your mother's circulation, your own circulation as a newborn, the drugs you're exposed to and your lifestyle. All those interact with genes even prenatally. We know genes get turned off or on prenatally depending on what the mother is exposed to, and even identical twins are not identical because of differences in circulation in different parts of the placenta.
So the disease we get is going to be combination of our background genetic susceptibility and lifelong exposure to variable environments. Really, every disease arises and manifests differently in each person, and one disease may well have different environmental origins or interactions. It's a huge challenge for medical education to convey this concept. But it's also a huge opportunity to have multiple places to intervene - in early diagnosis, to identify a susceptibility, change the environment, give environmental advice like diet and exercise or improve early screening.
OU Medicine: Speaking of environmental damage, you've studied the children of cancer survivors for signs that chemotherapy and radiation therapy affected them genetically. What have you found?
Mulvihill: We know the environment can change genes, but never has it been proved that any environmental agent has changed genes that manifest themselves as disease in the next generation through germ cell mutation. The Radiation Effects Research Foundation [for which Mulvihill is an adviser] hasn't seen it in 50 years of studying the children of A-bomb survivors in Japan.
We've taken (the question) up with another worst-case scenario of exposure that should hurt reproduction, namely cancer treatment. We know it breaks chromosomes and causes second cancers, so there is another informative, if unfortunate, cohort to study for possible origins of germ cell mutation. I have finished one study and am in the middle of another that merges some 14,000 kids born to cancer survivors and looks at them for the frequency of genetic disease. Contrary to expectations, we don't see any excess of cancer or genetic disease, narrowly defined.
The next big research goal is to look at the issue at the DNA level. It seems so likely that radio therapy or chemo therapy should change genes. How come we can't see it at the clinical level? Is there something about the human reproductive tract or gonads that repairs any possible damage before you'd get a useful egg or sperm? Wouldn't that be wonderful?
OU Medicine: Should each of us assume we have mutated genes?
Mulvihill: Yes, because after all, we know mutation occurs to fuel evolution. Mutation occurs. The present challenge is to see if we can relate it to a specific environmental exposure.
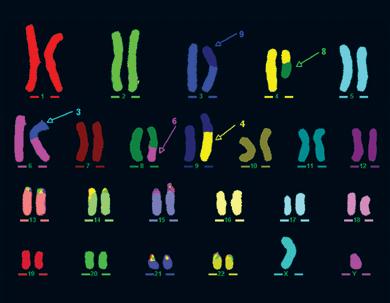
Because the OU Genetics laboratory
can pinpoint the precise site of translocations
in the test samples they receive, it is possible
to determine which genes are affected and
offer diagnoses. |
OU Medicine: More and more is learned about genetics every day. Where is this new knowledge taking us?
Mulvihill: Where we're going is to personalized, predictive and preventive medicine - PPP. That's what the director of the NIH talks about: Your predispositions to disease will be identified along with a recommendation for what you can do to overcome them - the special diet you should have, the special screening programs you should undertake. If you can't prevent the disease, you can predict and screen for it, and once a therapy is developed, make it highly personalized to minimize side effects.
OU Medicine: Should people with familial diseases like Huntington's consider genetic testing, even when there is no cure?
Mulvihill: Anyone - that's all of us - with genetic predispositions should ask the question, "Would I and my family benefit from gene testing?" We do see (children of) Huntington's patients and discuss testing with them. A fair amount decide they don't want to test. For me, the counseling is a success if they make a rational decision. Either choice is rational. Huntington's is in the family of a couple we're working with now. They're trying to decide whether they'll have children. Sometimes we see people when they've already had their kids, and they say, "I've got to know whether to change jobs. I'm not going to change jobs if I'm going to be limited in my work life. I'd better stick with my current job, which has insurance that will cover me when I get sick, versus taking a chance and switching jobs. If I'm going to lose physical function and insurance, that's not a risk I'm prepared to take, so I'd better have the test."
OU Medicine: What about women with breast cancer risk?
Mulvihill: Testing can change your screening behavior. My colleagues Debra Mitchell, M.D., and Melissa Kraft, Ph.D.,R.N., of Breast Imaging of Oklahoma, established a research protocol with three levels of risk - very high, high and moderately high. All patients got a mammogram; the next highest level got mammogram plus MRI; the women in the highest risk group also got ultrasound and MRI on a more frequent basis. Almost all (of the breast cancers found) in the four years of screening were in very high risk group. They were detected early and there were no deaths. In the large, moderate-risk group, only one breast cancer occurred, so the concept of risk-stratified screening seems to work.
OU Medicine: What diseases can someone be tested for?
Mulvihill: As of today, and it changes every week, there are 1,301 diseases (online at www.genetests.org) that can be tested for. Almost all are single gene diseases, such as neurofibromatosis and Huntington's, and 598 labs are testing. But what is a new area of controversy is that you can do a profile on yourself through companies that say, "Learn your genetics profile." Our professional societies are looking critically at the concept and feel there's not a role for a genetics profile for the average adult, certainly not without counseling and interpretation.
OU Medicine: When do you recommend testing for adults?
Mulvihill: We wouldn't screen everyone for colon cancer genes, for example, but we instead try to identify families that have a lot of colon cancer. If a mutation is found in one person, others in the family could elect to be tested for that mutation at low cost. If it's positive, family members have earlier, more effective screening or the removal of the colon before it becomes cancerous. There are choices to cope with genetic predispositions.
Another side of genetics is asking if there are determinants that alter your response to therapy. Does your cancer have a different metabolic or genetic origin that can change the drug that should be curative for your cancer? And do you have a certain way of handling certain blood thinners, so that the dose most people can tolerate will cause you an untoward reaction? The same dose is not sufficient for some people, and it causes excess blood thinning in others. This variation is caused by gene changes that can be tested for. So now the notion is being debated: shouldn't everyone on blood thinners be tested and put on the proper dose? Some say we're not getting into too much trouble by current practice.
OU Medicine: And for children?
Mulvihill: Newborn screening is expanding rapidly. Oklahoma was testing for 11 disorders before May, and by the end of the year it will be 49, using technology that screens for a lot of diseases at once. For instance, we screen for sickle cell anemia but pick up other hemoglobin disorders. I've been working on this for nine years with the Oklahoma State Department of Health - we've been wonderful partners in steering this through. This screening identifies likely metabolic conditions that, if left untreated, would cause the baby ill effects: sudden death, mental retardation or medical complications. Like cystic fibrosis - we wanted to screen for it because if you detect it at birth, the kids are healthier at 7 years of age.
What's happened in Oklahoma is credited to Pam King, R.N., recently retired as state genetics coordinator with the State Health Department, who insisted newborn screening be a program, an infrastructure to catch kids, and not just a lab test. Two of our employees, a nurse and a nutritionist, keep track of all these kids in the state from time they're born. A baby born in Altus, for example, would come here for confirmation of the diagnosis and early on would come back every other week. Once stability is achieved, the therapy would be in Altus. About 45 kids a year are recognized through this screening. It's anticipated that the additional screening will pick up 11 more.

|
Shibo Li, M.D., Director of OU Genetics
laboratory, goes over test results with
John J. Mulvihill, M.D.
|
OU Medicine: In addition to your two campus clinics for treatment and counseling, don't you also operate a next generation-class genetics laboratory?
Mulvihill: Yes, and the relationship between the clinics and the lab is a circle. We see patients, then (Lab Director) Shibo Li, M.D., suggests an appropriate lab test. He does the test, tells us what it means, we go to the patient or patient's family and deliver the interpretation and tell them what can be done.
Some cases are the first and only ones in the family, but we have to be alert to whether this has implications for the next baby or individuals in entire family. Just yesterday we had a patient who wondered if she had genetic predisposition for breast cancer because of a second cousin who tested positive. It turned out that she did. These two cousins, who hardly knew each other, now know they're connected by same gene and that at least eight other women in the family might be carrying it.
Because our equipment is so much better now, the lab is able to solve cases that couldn't be solved before, including cases that taught us new lessons on how genes are organized. For example is a case first diagnosed 15 years ago. The baby had what we call three-way translocation - where a part of one chromosome is patched to another and part of that one is patched to another and part of that one is patched to the first one - but we couldn't go to the next step and tie it all together. Dr. Li recently reanalyzed it, was able to find the exact places where chromosomes were broken, and because we can now look at a gene map of what genes are where, we were able to identify the problem as cleidocranial dysostosis. With the sophisticated technology we use, we're able to see more and more detail.
We have a patient now where something was wrong with her pregnancy. Her amniocentesis showed the baby had an extra copy of chromosome 17 in about 40 percent of his cells. It's called trisomy 17, akin to trisomy 21 for Down syndrome. Chromosome 17 is such a big chromosome that there's never been a live patient that has had trisomy 17 in all cells. It's probably just not compatible with fetal life. But this baby had just 40 percent mosaicism in the amniocentesis, which is basically the skin cells of the fetus. Blood was taken at birth, and a few cells had trisomy 17, but others had an unnecessary third copy of other chromosomes. We scraped cells from inside of the baby's mouth, and there was no abnormality in those cells. Neither parent had any abnormality. So how do you explain this? We don't know.
The current interpretation is that somehow or another, a genetic change messed up the normal segregation of chromosomes which ensures that daughter cells get exactly the right number each time. So is there a master gene that controls chromosome segregation? Wow! We'd never thought of that, but maybe so. And just one patient is teaching us that.
OU Medicine: It must be wonderful to be a physician-scientist at the frontier of such an exciting field.
Mulvihill: It's a privilege!