Adding a urogynecology procedure to a gynecologic oncology procedure is associated with minimal increased risk of adverse events. This data is helpful to guide counseling when considering treating pelvic floor disorders at the time of gynecology oncology procedures.
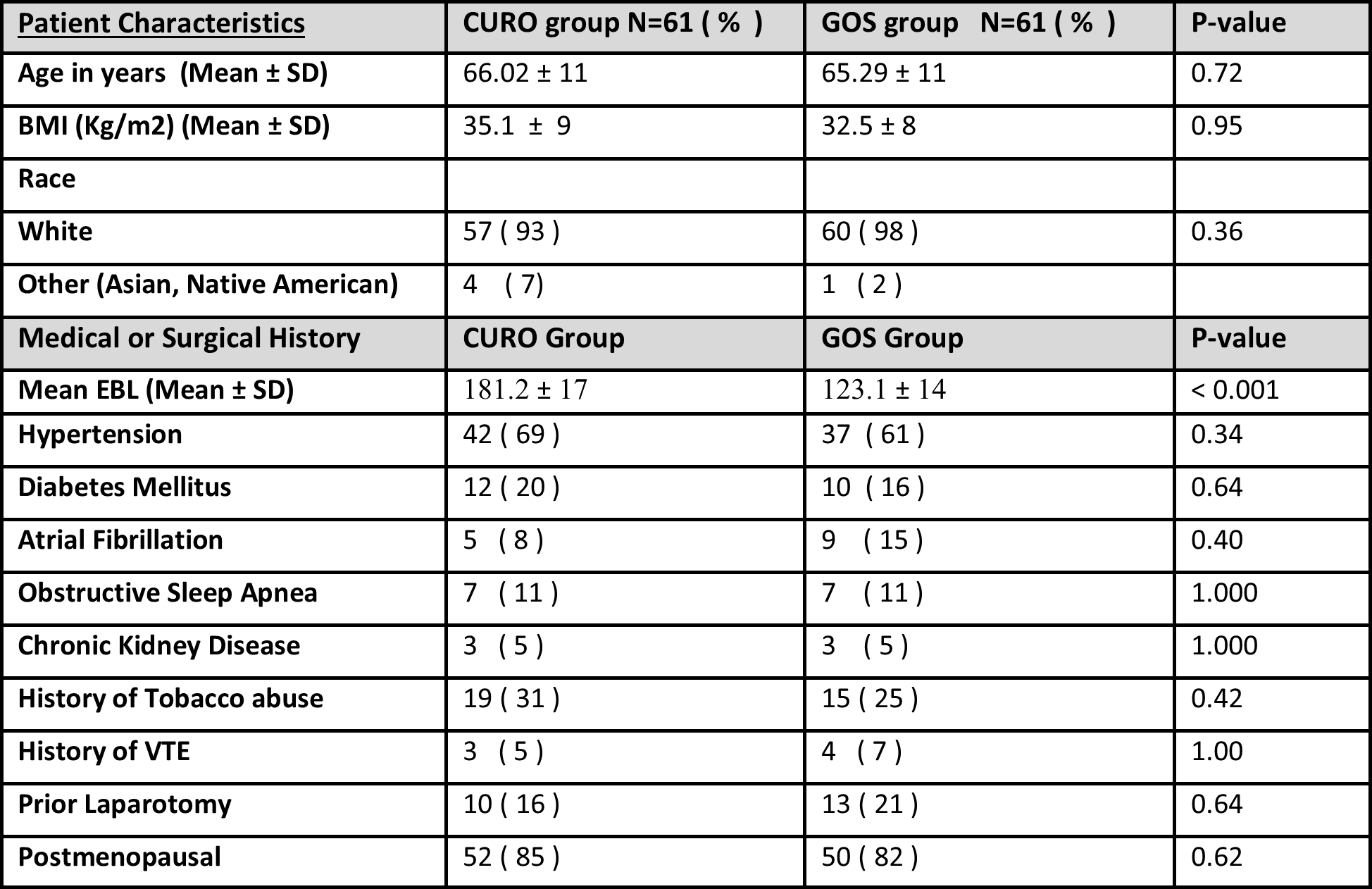
Table 1: Characteristics of concomitant urogynecology and gynecologic oncology patients. Patients grouped by Combined surgery (CURO) and Gynecology Oncology only surgery (GOS). Reported as N (%) unless otherwise specified. SD = standard deviation, BMI = Body Mass Index, EBL = Estimated blood loss, VTE = Venous thromboembolism